What is Endometriosis?
Endometriosis is a chronic condition in which tissue similar to the lining of the uterus, called the endometrium, grows outside the uterus. These growths may appear on the ovaries, fallopian tubes, bladder, intestines, or the pelvic wall. Like the normal uterine lining, these tissues respond to hormonal changes throughout the menstrual cycle—they thicken, break down, and bleed every month. However, because this blood has no way to leave the body, it becomes trapped, leading to inflammation, irritation, and the formation of scar tissue or adhesions that can bind pelvic organs together.
Endometriosis is one of the most common gynecological conditions, affecting about one in ten women of reproductive age. Despite being common, many women remain undiagnosed for years, as its symptoms are often mistaken for other conditions such as ovarian cysts or pelvic inflammatory disease. It is not a malignant disease, but its impact on a woman’s life can be profound, causing chronic pain, heavy periods, and fertility problems.
Early diagnosis and treatment are crucial for managing symptoms and preventing complications. Treatment varies depending on the severity of the condition and the woman’s desire for future pregnancy.
Causes of Endometriosis
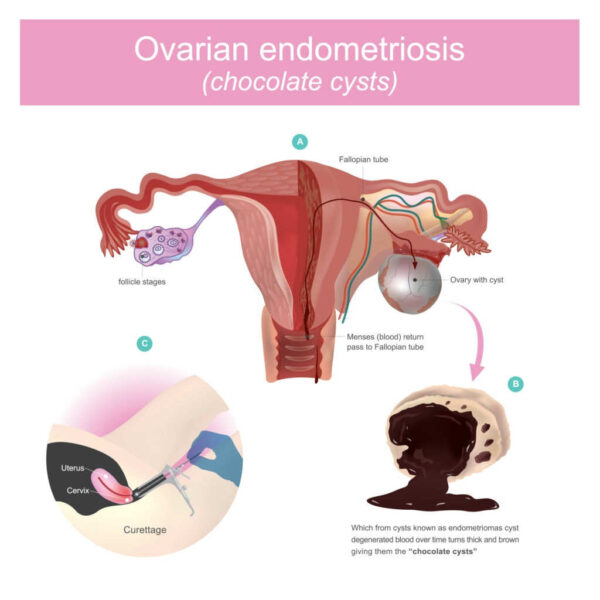
The exact cause of endometriosis is still not fully understood, but several theories attempt to explain its development. The most widely accepted explanation is retrograde menstruation, which occurs when menstrual blood containing endometrial cells flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body. These cells then attach to the pelvic walls or organs, grow, and continue to respond to hormonal changes each month.
Another theory suggests that genetic factors play a role, as the condition tends to run in families. Women who have mothers or sisters with endometriosis are more likely to develop it themselves. Immune system dysfunction is also believed to contribute, since a weakened immune system may fail to recognize and destroy misplaced endometrial tissue.
Some researchers believe that hormonal imbalances, particularly high levels of estrogen, may stimulate the growth of endometrial-like tissue outside the uterus. Additionally, embryonic cell transformation could be involved, where cells in the abdomen convert into endometrial cells during puberty under the influence of hormones.
Other possible factors include surgical scars, such as those from a cesarean section, which may allow endometrial cells to attach and grow, and environmental toxins, like dioxins, which may disrupt hormonal balance and immune responses.
Common Symptoms of Endometriosis
Symptoms can vary greatly from one woman to another. Some experience severe pain, while others have mild or no symptoms at all. The most common signs include:
-
Pelvic pain, especially during menstruation, which is often more intense than typical period cramps.
-
Pain during intercourse, particularly deep penetration.
-
Pain during urination or bowel movements, especially during menstruation.
-
Heavy menstrual bleeding or bleeding between periods.
-
Fatigue, bloating, nausea, or digestive disturbances such as diarrhea or constipation during periods.
-
Difficulty getting pregnant, as endometriosis is one of the leading causes of infertility in women.
The severity of symptoms does not always reflect the extent of the disease. Some women with extensive endometriosis may feel little pain, while others with only a few lesions experience significant discomfort.
Complications of Endometriosis
The most serious complication is infertility, which affects up to half of women with the condition. Endometriosis can damage the ovaries and fallopian tubes, interfere with the release of eggs, or prevent fertilization and implantation.
Another complication is the formation of ovarian cysts, known as endometriomas, which can rupture and cause severe pain. Adhesions and scar tissue may also distort pelvic anatomy, leading to chronic pelvic pain even outside menstrual periods.
In rare cases, endometrial tissue can spread beyond the pelvic organs, affecting areas such as the lungs or diaphragm, leading to chest pain or breathing difficulties during menstruation.
Diagnosis of Endometriosis
Diagnosing endometriosis can be challenging because symptoms mimic many other conditions. The process usually begins with a detailed medical history and a pelvic examination to check for abnormalities.
Imaging tests such as ultrasound and MRI can help identify cysts or lesions, but the only way to confirm the diagnosis is through a laparoscopy—a minimally invasive surgical procedure in which a small camera is inserted through a tiny incision in the abdomen to view the pelvic organs directly. During laparoscopy, tissue samples may be taken for biopsy to confirm the presence of endometrial cells outside the uterus.
Treatment Options for Endometriosis
Treatment depends on the severity of symptoms, the location of the lesions, and whether the woman wishes to become pregnant. There is no permanent cure, but various approaches can help control pain and slow disease progression.
1. Medications:
-
Pain relief: Over-the-counter painkillers like ibuprofen or naproxen help reduce menstrual pain.
-
Hormonal therapy: Hormonal treatments, such as birth control pills, progesterone therapy, or gonadotropin-releasing hormone (GnRH) agonists, can suppress ovulation and limit the growth of endometrial tissue.
-
Aromatase inhibitors: These drugs lower estrogen production, which may help in severe cases resistant to other treatments.
2. Surgery:
For women with severe symptoms or infertility, laparoscopic surgery can remove or destroy endometrial implants and scar tissue while preserving the uterus and ovaries. In advanced cases where pain persists and fertility is not a concern, hysterectomy (removal of the uterus) may be considered, sometimes along with removal of the ovaries.
3. Assisted reproductive techniques:
If pregnancy is desired but natural conception is difficult, options such as in vitro fertilization (IVF) can increase the chances of success.
4. Lifestyle and supportive care:
Regular exercise, maintaining a healthy weight, managing stress, and following an anti-inflammatory diet rich in fruits, vegetables, and omega-3 fatty acids may help relieve symptoms.
Living with Endometriosis
Endometriosis can take a toll both physically and emotionally. Chronic pain and fertility struggles often lead to frustration, anxiety, and depression. Emotional support, whether through counseling, support groups, or open communication with a healthcare provider, is essential for improving quality of life.
Many women find relief through a combination of treatments, and with proper medical management, most can lead healthy and fulfilling lives. Early recognition and intervention remain key to preventing complications and maintaining fertility